Mayo Clinic researchers say they have found the cause of most chronic sinus infections -- an immune system response to fungus. They say this discovery opens the door to the first effective treatment for this problem, the most common chronic disease in the United States.
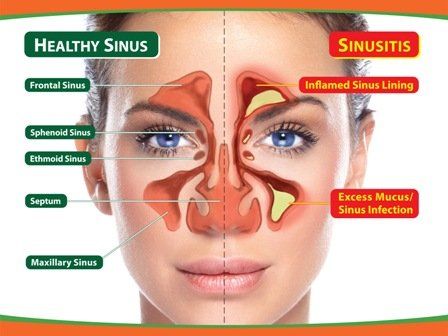
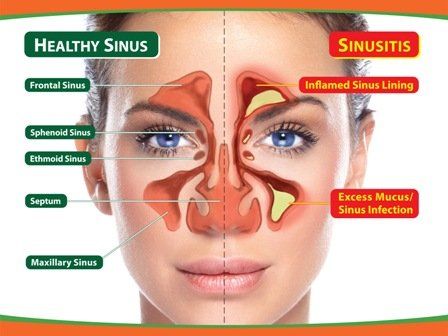
An estimated 37 million people in the United States suffer from chronic sinusitis, an inflammation of the membranes of the nose and sinus cavity. Its incidence has been increasing steadily over the last decade. Common symptoms are runny nose, nasal congestion, loss of smell and headaches. Frequently the chronic inflammation leads to polyps--small growths in the nasal passages which hinder breathing.
"Fungus allergy was thought to be involved in less than ten percent of cases," says Dr. David Sherris. "Our studies indicate that, in fact, fungus is likely the cause of nearly all of these problems. And it is not an allergic reaction, but an immune reaction."
Mayo Clinic Study Implicates Fungus As Cause Of Chronic Sinusitis. Science Daily, 10 September 1999. Read the press release.
Another important component of chronic sinusitis is biofilms.
What are Biofilms?
Bacteria, fungi and yeast exist in two forms: (1) free floating organisms called planktonic forms and 2) sessile forms known as biofilms.
The biofilms are an adaptive phenotypic switch that occurs in bacteria, fungi and yeast. Biofilms are the main mode of survival and proliferation of these micro organisms. The biofilm is an extracellular matrix (ECM) consisting of polysaccharides, nucleic acids, proteins and extra-cellular DNA (Tamashiro et al, 2009; Loussert et al, 2010; Nailis et al, 2010).
The biofilm is 90 % water and 10 % ECM and cells. The ECM is porous, allowing nutrients to penetrate the biofilm and to permit waste excretion. Ironically, the biofilm protects the cells within the ECM from shear-gradients, antibiotics, antifungals and the innate and adaptive host defenses.
Treatment of chronic fungal and bacterial rhinosinusitis with antifungals and/or antibiotics kills off the planktonic organisms, while leaving the biofilm organisms essentially untouched. Thus, chronic flare-ups of the sinusitis recur (Tamashiro et al, 2009; Mowat et al, 2008; Singhal et al, 2010).
The frequency of biofilms in chronic fungal and bacterial sinusitis patients ranges from 50 to 90%, depending on the diagnostic protocol (Foreman et al 2009, 2010). The organisms most often associated with chronic rhinosinusitis are Staphylococcus aureus, Haemophilus influenzae, Pseudomonas aeruginosa and a variety of fungi including Aspergillus fumigatus (Foreman, Wormald PJ 2010; Chakrabarti et al, 2009). However, a variety of aerobic and anaerobic bacteria have also been reported (Brook, 2006).
Current efforts are being directed toward the efficacy of various treatments to penetrate and break down the biofilms.
So far, N-acetylcystein has been shown to break down the adhesion properties of biofilms (Pintucci et al 2010). While in a sheep model, regular treatment with mupicron produced a marked reduction in the biofilm surface area (Le et al, 2010).
It is apparent that a concerted effort is needed to reduce recurrent exacerbations that are associated with biofilm protection of infectious agents.